-
Australia
Copyright © 2026 Powered by BCI Media Group Pty Ltd
Confirm Submission
Are you sure want to adding all Products to your Library?
Contact Detail
18 Nov 2021 by Enware

Legionella is a lingering, ever-present bacterium which, in the right breeding conditions poses a significant health risk.
The disease causing bacteria found in potable water supplies is spread when people inhale in a mist or vapour – from air conditioners, showers and heated water systems. Undetected, Legionnaires’ disease can lead to severe illness and potentially death, particularly for people in high risk categories, such as the elderly or those suffering with cancer, diabetes or a chronic lung disease who often have a weakened immune system
Hospitals are one of the highest risk environments for Legionella as they have large and complex water systems coupled with the vulnerability of those using it therefore detailed water management is crucial to avoiding outbreaks.
Preventing an outbreak is an ongoing and complex process. Although routine maintenance, record keeping and risk management plans are already required as part of the relevant Codes of Practice, Public Health Acts, and Australian Standards for each State, system design and fixture choice can significantly impact prevention control.
This whitepaper examines the impact of Legionnaires’ disease on public health and the impact current water system design in Australia can have in encouraging bacteria to breed. It will also look at how the issue is being tackled internationally, and what technology advancements allows for effective disinfection, easier maintenance, and a greatly reduced risk of Legionella.
“ Preventing an outbreak is an ongoing and complex process... system design and fixture choice can significantly impact prevention control
Outbreaks of Legionnaires’ disease have created national and worldwide public concern, particularly because of the ease at which an outbreak can occur and its insidious mode of transmission.
As recently as February 2015 in New York, a Legionnaires’ outbreak resulted in the death of 12 people and left at least 100 others infected, when the disease made its way into hotel cooling towers1.
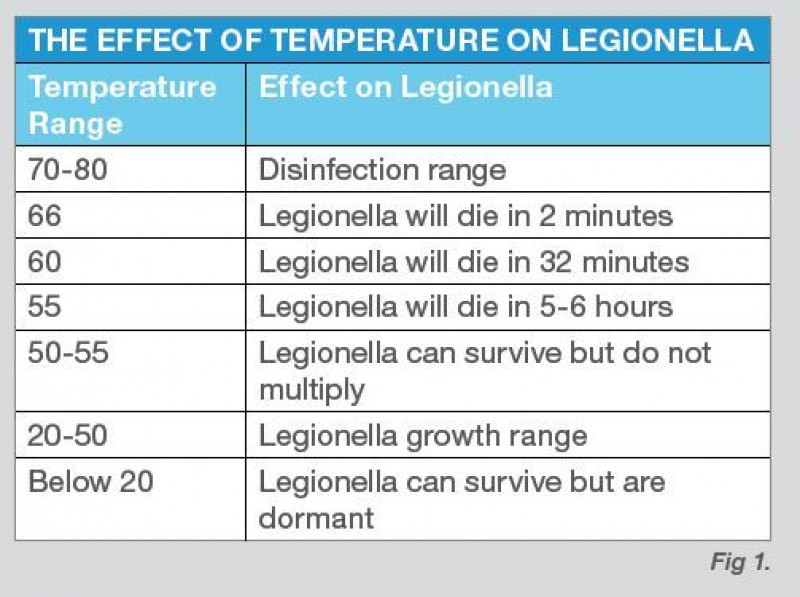
Closer to home, this event reminds us of one of Australia’s biggest outbreaks in 2013, when contaminated warm water drawn through hospital taps at Brisbane’s Wesley Hospital resulted in the death of a patient and left another critically ill in intensive care2. It was reported that a State Government energy efficiency program may have increased the risk of Legionella bacteria growing in water supplies. Temperature controls in place at the hospital meant water could not reach a temperature higher than 45ºC. This created an optimum birthplace for bacteria growth as Legionella flourishes at temperatures between 25ºC and 45ºC3.


The Plumbing Code of Australia (NCC Volume 3 – 2015) requires heated water be stored and delivered under conditions which avoid the likelihood of the growth of Legionella bacteria. The National Plumbing and Drainage Code4 stipulate hot water be stored at no less than 60ºC to help prevent the growth of Legionella.
However these temperatures can cause scalding, so water temperature is required to be controlled in accordance with AS/NZS3500.4. This standard currently states that in healthcare facilities the only deemed to satisfy solution is through the use of thermostatic mixing valves set to a maximum temperature of 45°C. However, some State health departments have created their own Policy Directives which have allowed centralised whole of building distribution of warm water despite these systems having no current recognition or clear design guidelines within the Plumbing Codes in force in Australia.
Stagnation is another key breeding factor that will exacerbate Legionella growth in water systems. When
water is used infrequently or where there are significant dead legs in pipework, the risk of contamination is increased. It is both good design practice and the requirement of various State Health guidelines to reduce the length of warm water pipework in order to minimize dead legs, and in some circumstances to remove them completely as well as ensuring systems are flushed on a weekly basis when taps have not been in use. (Guidelines for the control of Legionella SA 2013)
In the case of Brisbane’s Wesley Hospital managing the outbreak was not easy. A full scale Public Health unit investigation into the hospital’s cooling and water systems, as well as independent sampling and investigations found the source of contamination was the heated water system. Contributory factors to the harbourage of Legionella were identified in the presence of dead legs, and a lack of awareness regarding the need for regular and on-going maintenance of plumbing fittings.
Following the incident, Queensland Health asked almost 250 state and private hospitals to test their water systems for Legionella. The results indicated the extent of Legionella in water systems, with at least a quarter of all hospitals tested returning a positive result5.
If we are well aware of the risks associated with water temperatures and current hydraulic designs, then why is so little being done about it?
Warm water lines have become an ingrained and accepted element of hydraulic design in Australia. However, with most warm water circulating at temperatures between 40ºC and 50ºC Legionella is being giving the best possible chance to thrive. In the long and complex piping systems of hospitals dead-legs are especially prevalent and contamination can easily occur.
Whilst internal water systems in Australia have traditionally been designed with issues such as Legionella control in mind, but with minimal design guidelines and inconsistency between States and other various bodies who have regulatory ownership in this space conflicts can occur!
Additionally, views on effective water treatment processes also vastly differ. Disinfection systems using UV (Ultra Violet), chemical dosing and thermal disinfection have shown to have limited effectiveness. When combined with a lack of design regulation and consistency facility owners and managers are being left with expensive and confusing processes to ensure healthy water quality compliance is attained.
Australia’s slow response and inconsistent views on the issue of Legionella control in water systems is in high-contrast to aligned markets such as the UK and major parts of Europe such as Germany. UK and Europe are leading the way in the management of Legionella in hospitals, with the UK Department of Health providing comprehensive advice and guidance in a code of practice for the control of Legionella in health water systems.
Critical practices stated include:
These practices are focussed around keeping water hot at all times. Keeping water hot at all times requires a device for safe delivery and avoiding potential scalding is of serious concern.
For safe delivery, thermostatic mixing valves which mix hot and cold water at the point of use ensuring the water can be kept hot for as long as possible, without the risk of scalding.
It is preferable that thermostatic mixing devices are fitted directly to the outlet, or be integral with it, and be the method of temperature and flow control.


The ongoing threat of Legionnaire’s Disease is a very real one and something which must be addressed by the building and design sector.
There is a responsibility for those entrusted with the design, construction and maintenance of Australian hospitals and aged care facilities to challenge the status-quo in relation to the hydraulic systems used.
There is a need to eradicate warm water lines to fully minimise the risks of Legionella forming in the water supplies of our hospitals and aged care facilities. This is supported by various State Health Departments regulations, yet the design integration of these new technologies is slow. The use of new technologies must be explored and implemented if Australia is to avoid falling even further behind the rest of the world in managing bacteria and looking after our most vulnerable.
While these new technologies may appear, to some, to have an initial greater capital cost, they will help with a significant reduction in service and maintenance costs, greater risk minimisation and long-term cost savings.
Enware Australia has developed the first point-of-use sequential Thermostatic Mixing Valve (TMV) range purpose designed for high risk applications such as hospitals and aged care facilities. This technology offers superior scald protection as well as water and energy-saving features.
By integrating the thermostatic mixer into a pointof-use mixer, the risk of Legionella is minimised as full temperature heated water is plumbed directly to the draw off fixture eliminating warm water pipe lines where Legionella may breed.
A sequential thermostatic mixer, works by blending hot and cold water at the point of use to ensure a stable, constant desired temperature ( typically in a range from 38ºC to 43.5 ºC) at wash basins, showers and bathtubs to prevent scalding or user discomfort. In addition it delivers both water and energy efficiencies beyond those of traditional tapware and thermostatic mixer combinations, minimises dead-legs in pipework, allows for easier hot water disinfection of systems, and has a self-draining design which further reduces bacteria growth risk.
Enware strives to provide the health care industry with solutions that enhance safety whilst at the same time improving performance and efficiency. A transformation in design thinking from behind the wall multi point thermostatic mixing valves to point of use is proven to drastically minimise risk for healthcare water systems.
To address these needs, Enware has developed the Aquablend™ SQX Sequential Thermostatic Mixers and eSQX Touch Free Thermostatic Mixer.